Key points to know:
- Burning mouth syndrome is a diagnosis of exclusion – made when no other diagnosis fits.
- People with burning mouth syndrome don’t usually have anything visible in their mouth, like sores or rashes, but some do.
Burning Mouth Syndrome Diagnosis
It is hard to get a burning mouth syndrome diagnosis. The diagnosis is made through a clinical evaluation of your mouth and by ruling out other conditions that could be causing the burning pain. This is called diagnosis of exclusion. If they can’t find something to cause the pain, it is likely burning mouth syndrome.
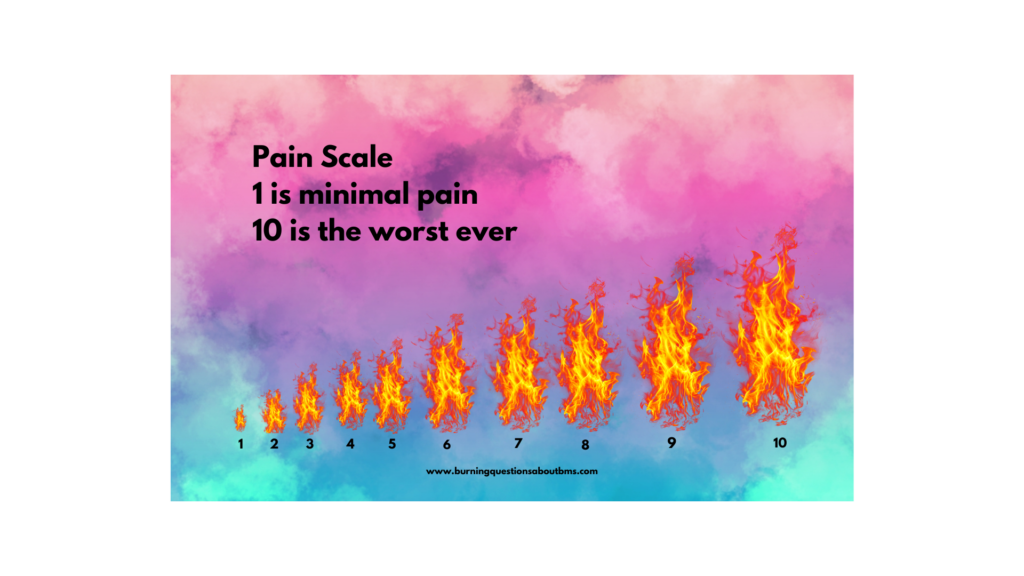
Dentists, physicians, nurse practitioners, and physician associates can do an examination to see if they can find something that might cause secondary BMS. If you can though, it’s best to see an oral medicine specialist or an oral and maxillofacial pathologist. You’ll be asked to describe the pain. You might be asked to rate it on a scale of 1 to 10, with 1 being minimal pain and 10 being the worst you can imagine.
They would look at your mouth to check for lesions, sores, or anything unusual on the oral mucosa. They may take swabs if they believe there might be an infection. If you take any medications, they might recommend switching to another to see if the pain is a side effect. Other possible tests include:
- Salivary flow measurement
- Blood tests
- Allergy tests
- Head and neck imaging studies (x-rays, MRI)
- Gastric reflux tests
- Biopsy of the oral mucosal tissue
If they don’t find anything, the diagnosis might be primary BMS.
Getting a diagnosis is just the first hurdle. Unfortunately knowing that you have burning mouth syndrome likely won’t lead to instant pain relief. Your specialist may offer different treatments for you to try but each person’s journey with BMS is different. What might work for one person won’t necessarily work for another.